Diving into the world of solid food with your baby is a messy, adorable milestone that, let’s be honest, sometimes feels a little confusing. While some little ones happily slurp down baby cereal at 6 months, others won’t go near a mashed carrot until they’re hitting the 9-month mark — what gives?
The truth is, while solid food exposes babies to new tastes and textures, it’s not even necessary in the very beginning (yes, really).
“While the general recommendation for starting solids is between 4 and 6 months old, solids at this point are more about introducing baby to new tastes and developing oral motor function,” says Dr. Melanie Custer, a pediatrician at Deaconess Clinic in Evansville, Indiana. “Breast milk or formula should continue to be the primary source of nutrition through 12 months.”
Of course, when your baby is eyeballing your bowl of oatmeal every morning, it’s only natural to start wondering when to start baby food. Here, experts and veteran parents weigh in on the dos and don’ts of starting solids, a.k.a. Stage 1 foods. Ready the bibs!
What is Stage 1 baby food?
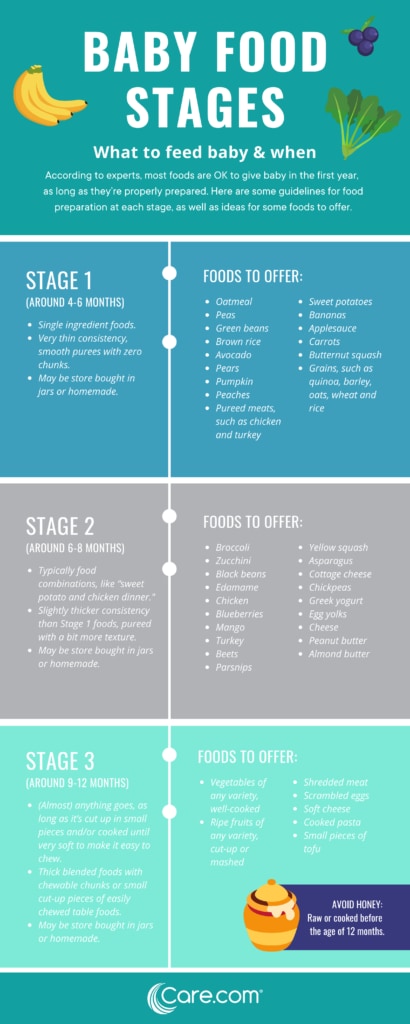
Stage 1 foods are single-ingredient foods that are very thin in consistency. You can either buy them at the store or make them yourself, as long as they’re a smooth puree with zero chunks and include just one ingredient so you’re introducing your baby to one new food at a time.
And remember, every child is different and develops at their own individual pace. Check with your child’s doctor for baby food recommendations during the first year.
When to start Stage 1 baby food
According to Custer, the reason it’s recommended that full-term babies wait until 6 months to try solids is because they’re losing iron stores that were built during pregnancy, and iron is important for infants’ brain development.
“Growing babies need all the nutrients they can get — and breast milk and formula are both far superior to solids when it comes to nutrients, including iron,” says Jenifer Thompson, an advanced practice dietician at Johns Hopkins in Baltimore. “It’s important to remember that solid foods are also called complementary foods because their intention is to complement the breast milk and/or formula baby is drinking.”
Thompson also notes that offering solids too early on — prior to 4 months — has been associated with excessive weight gain and adiposity (excess fat) in preschool and older ages.
Signs baby is ready to start solid food
Knowing your baby is ready for Stage 1 foods goes beyond celebrating their half-year birthday. It’s important to look out for developmental and social signals, as well.
“One of the biggest indicators that your baby is ready for solid foods is that they’re showing an interest in what other family members are eating,” says Dr. Kristen Treegoob, a pediatrician at Children’s Hospital of Philadelphia.
If you notice baby staring at your food and opening their mouth or leaning forward if food is ever offered, these are signs that solid foods have piquéd your baby’s interest, according to Thompson.
“I knew my son was ready for solids when, at 7 months, he started staring — like, really staring — at all of our food during dinner,” says mom of two Erin Henderson, of Waltham, Massachusetts. “It reached a point where we felt bad eating in front of him!”
Other signs your baby may be ready for solids, according to Custer and Thompson, include:
- They can sit up with little to no support.
- They can hold their head up without being wobbly.
- Their tongue thrust reflex has disappeared. “Before introducing solids, it’s important to make sure your baby can open their mouth for a spoon and accept food off of it, rather than pushing it away with their tongue, which is an involuntary habit until about 4 months,” says Custer.
What Stage 1 baby food to start with
According to Thompson, it’s recommended that early solid foods provide a source of iron, protein and zinc. But remember, you’re complementing your baby’s diet, not revamping it, so it’s OK to get a little creative and go with your gut.
“There is no medical evidence that solid foods must be introduced in any particular order, or that vegetables must be introduced before fruits to ensure that they don’t have a preference for sweets and will it not lead to a dislike of vegetables,” says Thompson.
And once you get going, continue to mix it up.
“There is no one-size-fits-all for solid food introduction, and we typically recommend parents introduce a variety of tastes, colors and food groups in the first few months,” says Treegoob. “That said, the American Academy of Pediatrics recommends that breastfed infants first begin with iron-rich foods, which include iron-fortified infant cereals and iron-rich pureed meats. Formula-fed infants typically get enough iron through formula, so they may have a little more flexibility at first.”
Here’s a list of first foods to try (make sure all are pureed to very thin consistency):
- Bananas.
- Avocados.
- Sweet potatoes.
- Carrots.
- Pureed meats, such as chicken and turkey.
- Butternut squash.
- Peaches.
- Applesauce.
- Grains, such as barley, oats, wheat and rice.
Custer does note that infants should not eat raw or cooked honey until 12 months, as it might contain spores that can cause infantile botulism, a serious illness that can hamper an infant’s ability to move, eat and breathe. For more tips on food storage, our experts weigh in on how long baby food lasts.
How to safely start Stage 1 infant food
When your baby first starts experimenting with solids, keep in mind it’s a gradual process, and you’re still a ways off from three solid meals per day. In the beginning, it’s best to think of solids as more of a snack than a meal.
“Babies will often start with just a bite or two at first and advance to three to four tablespoons at a time,” says Custer. “When they’re first starting off around 6 months, they can have solids one or two times a day.”
“Babies will often start with just a bite or two at first and advance to three to four tablespoons at a time.”
— Dr. Melanie Custer, pediatrician
“Foods should be offered one at a time when babies are starting off with solids,” says Thompson. “Then, wait between three to four days before introducing a new one, so you can properly identify an adverse reaction or intolerance.”
Here are a few more tips for feeding your baby Stage 1 foods:
- Make sure they’re sitting in an upright position, such as in a highchair, to prevent the risk of choking.
- Add a little breast milk or formula to their food. “At first, foods should be just slightly thicker than breast milk or formula to allow the infant to get used to eating,” Custer says. “Foods can get thicker as their eating skills are mastered.”
- Always feed your baby with a spoon. “Unless you’ve been advised by your pediatrician, never put solid foods, including infant cereal, in bottles with or without milk,” says Treegoob.
- Give baby breast milk or formula first. “Both of my babies were more open to trying solid foods in the beginning when they were happy and relaxed,” says mom of two Darcy McConnell of Garwood, New Jersey. “That was always after they had their bottle.”
Also, be patient. Starting solids is a learning curve for everyone.
“If your baby turns their head away, spits out food or pushes you away with their hands when you try to feed them solid food, then they are not quite ready,” says Treegoob. “Try again in a few days.”
“If your baby turns their head away, spits out food or pushes you away with their hands when you try to feed them solid food, then they are not quite ready.”
— Dr. Kristen Treegoob, pediatrician
How baby-led weaning works
Another way to start your baby on real food is baby-led weaning, which forgoes what’s thought of as Stage 1 baby food altogether, as well as a spoon.
“The baby-led weaning approach to introducing solid foods recommends that purees and traditional baby foods be omitted, and to start with finger foods, as well as self-feeding right from the beginning,” says Thompson. “This method may be preferred for some, but should always be discussed with a pediatrician since a possible concern of this method is the risk of choking, which could be minimized with appropriate food choices.”
Proponents of baby-led weaning believe that letting baby pick, choose and explore food on their own will help with appetite control overall (possibly reducing the risk of obesity later in life), as well as promote a taste for a wider range of foods. All of this said, research on baby-led weaning is still fairly scant, so it’s important to discuss it with your pediatrician if you choose to take this approach.


